Ecosperity in brief: 3 Ways data is saving your life
They monitor hearts, count calories and steps and track your sleeping patterns. But for all the hype, are wearable tech and other data-driven devices actually having any effect on our lives?
At our recent Ecosperity conference, a panel of experts comprising geneticist and CEO of life sciences research outfit Verily Andrew Conrad, prominent American surgeon Mark Ott and healthcare venture capitalist Michael Greely, discussed how ‘life-logging’ data and tracking technologies are helping ordinary individuals live healthier, more productive lives:
 From left: Dr Stephen Oesterle, Temasek Corporate Advisor; Dr Andrew Conrad, CEO, Verily; Michael Greeley, General Partner, Flare Capital; Dr Mark Ott, Central Region Regional Chief, Medical Director
From left: Dr Stephen Oesterle, Temasek Corporate Advisor; Dr Andrew Conrad, CEO, Verily; Michael Greeley, General Partner, Flare Capital; Dr Mark Ott, Central Region Regional Chief, Medical Director
Saving Blood — and Lives
If you had to go for surgery, you’d want to pin your life on a vastly experienced surgeon. It’s true — the more experienced the surgeon, the better for you, the patient. Now, that logic holds only in the absence of data. Information, not experience, may soon be the superior decision-making tool.

Take the tricky task of blood transfusions during surgeries, for example. With more transfusions, the risk of infection increases rapidly, and the amount of blood used in surgeries varies wildly, dependent almost entirely on the surgeon.
At the Intermountain Healthcare group of hospitals in the U.S Mountain States of Utah and Idaho, information is collated from surgeries using data-tracking technology to pinpoint how blood is used during transfusions.
The blood usage analyses are then periodically emailed to the hospitals’ surgeons and compared — without judgement — to existing best practices. Over time, the units of blood used has decreased by a third, saving about USD 2.5 million a year, and post-operative infection and one-year mortality rates also decreased substantially.
The beauty of it all? The surgeons were able to act on the information provided, but they didn’t feel coerced into action. They could decide what to do with it, and retained complete control over what was valuable to their patient.
Track Your Health With Every Teardrop
These days, nearly everyone has some kind of data tracker available to them — most mobiles have at least one tracking application built into them. As tracking technology becomes mainstream, wearable tech is getting smaller, less costly and increasingly able to supply information in real-time.
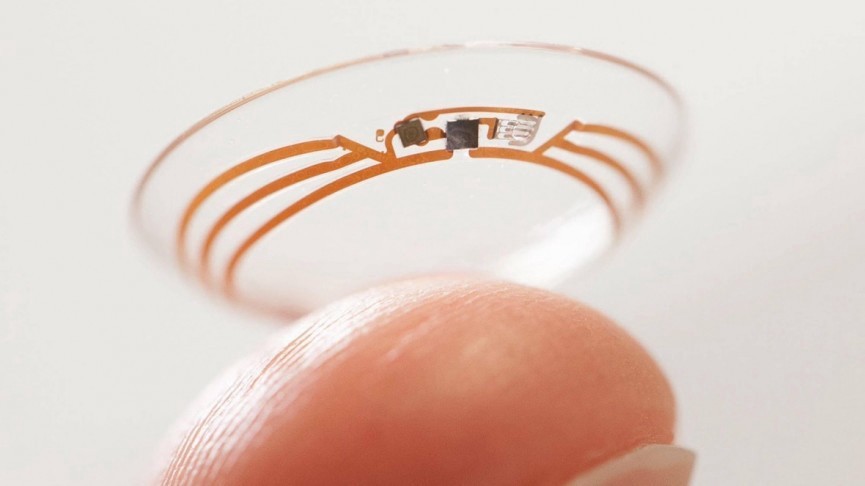 Photo: Verily
Photo: Verily
On that note, Verily is developing a contact lens that has a sensor embedded within it that will measure the level of glucose in your — get this — tears. Diabetics wearing the lens will be able to track, in real time, the effect of different foods on their glucose levels. Now imagine putting a doughnut in your mouth and seeing the resulting spike it has on your glucose levels even if you aren’t diabetic!
This wearable eye tech also eliminates the painfully laborious process of food journalling (logging what you eat), and allows patients to effortlessly transfer accurate, concise data to their physicians.
Putting the patient in charge — with smart technology
Ask anyone who has spent time in a public hospital — doctors, nurses, support staff — and they will tell you that they’re overworked and understaffed. For patients recovering from surgery, this can mean that they don’t get to walk as much as they should to recover properly.

Here’s what Intermountain Healthcare did: it incorporated a ‘smart’ recovery programme, provide monitors reminding patients to walk, tracked how much they walked, and fed this information back to their physicians and themselves. The result? Patients averaged more than 1.5 kilometres each on the first day after surgery — an astounding improvement achieved simply by shifting the responsibility from nurses to patients themselves.
Even better news: all the post-operation walking led to patients being discharged sooner, and fewer of them developing post-operative complications. Re-admission rates were also cut by half. Not only did patients benefit, but the hospitals also saved costs and freed up their nurses to perform other tasks.

So clearly, data has immense potential but it continues to be underutilised in the healthcare industry. Incorporating smart wearable sensors into patient care could augment physician-patient relationships, empower patients to take charge of their own health, and transform healthcare management and spending. On a grander scale, with more people using tracking technology the compiled data could lead to new insights into particular diseases and better treatment plans. Now that’s a data point that should not be lost on us all.